

As a Junior Surgical Resident at Massachusetts General Hospital we had a rotation through Lynn Hospital.
I had just come up from my Shock Trauma Internship at the University of Maryland. A 55 year old male presented to the Emergency Room with a severe heart attack.
Back in the early 70s, people routinely died from heart attacks in community hospitals. There were no cardiac catheterization services, CAT scans, MRIs, sonograms. There was only one trauma center in the entire country! I just came from it, at the University of Maryland. Open heart surgery was in its infancy. During my rotation in open heart at University of Maryland in 1973, mortality was 80% and worse at other times!

CPR failed, the medical crew could not stabilize him and when he went flat line, I performed the two minute ballet with no gloves as a last chance. Time was of the essence. Count down from the clavicle like a pianist. Two sweeps of a #10 blade staying away from the lower margin of the rib which has a groove containing the blood vessels. Push the lung aside and open the pericardium. Upon squeezing the heart, it started right up giving us time to administer medications and oxygenation. Then off to the operating room to close the wound.
At first I was so excited! I had saved a life in no uncertain terms. I beat the Grimm Reaper! I pulled off the two minute ballet flawlessly. I was hot shit!
After a few days it became evident that we saved the body, but not the brain. The patient could not remember his wife or the past. It gave me pause. Was it worth it? Should I have let nature take its course? I left that rotation without ever knowing the long range outcome of that reflex decision. It was sobering. It shook my foundation.
This skill set, however, served me well in the Emergency Room and Operating Room over the next years of residency. Dozens of gunshot and stab wounds to the heart and pulmonary arteries and veins received a second chance in life by fast and decisive treatment.
Then finally, late in my surgical training, those skills and expertise intersected my date and time with destiny. But that is another story.
Part two of three.
REALITY CHECK
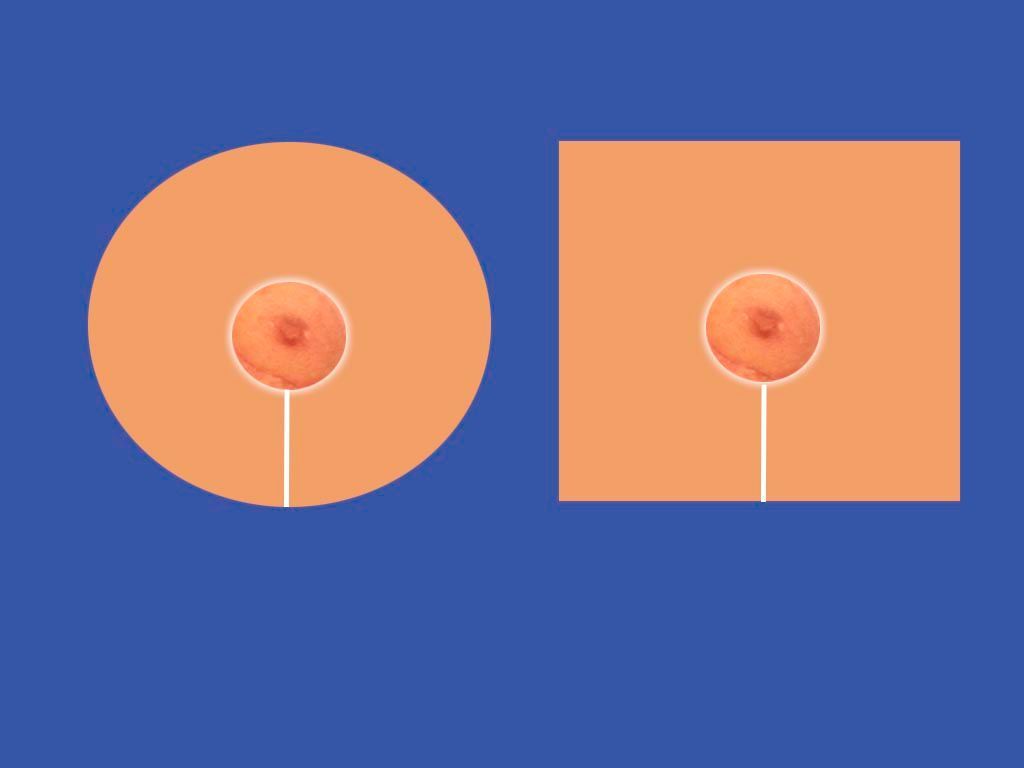
No matter how meticulous the technical mastery of the surgery, which is totally under control of the surgeon, there comes the healing phase which has a mind of its own. Every patient heals differently depending on the mysteries of their genetic code.
The best we can do is set up the conditions for optimal healing, (delicate tissue handling, tissue plane dissection, atraumatic suture techniques, drains, dressings, etc.) and the rest is up to nature.
Identifying potential complications early (hematomas, cellulitis, hypertrophic healing, allergic reactions, etc.) and dealing with them before they progress to disasters requires checking the patient the day after surgery now that in-hospital observation and recovery is unaffordable.
We have seen some rare but crazy anomalies and fortunately had the training and experience and luck to deal with them without worsening the condition.
We are based in:
421 SE Osceola St.
suite A Stuart,
FL, US 34994
Call us:
Email us:
All Rights Reserved | Villar Plastic Surgery | Privacy Policy